Workout pain, medical PTSD and pain management tips

Topics
Welcome to the Dr. B Newsletter, a curated healthcare email that delivers vetted reads on whole-body health. It’s hard not to feel alone when we’re struggling with pain. “The merest schoolgirl, when she falls in love, has Shakespeare, Donne, Keats to speak her mind for her,” Virginia Woolf once penned. “But let a sufferer try to describe a pain in his head to a doctor and language at once runs dry.”
This week, we devote a few words to pain—its presence, validity and limited control. Here’s hoping a little more knowledge + intention can help us reclaim our power over it.
- The Checkup: the struggle is real
- Ow! pain doubt + PTSD + working out
- Healthcare: Medicare + immunity
- We Now Treat: high cholesterol!
The Checkup
- How norovirus spreads through food + what to watch for
- Hayden Panettiere opens up about addiction + postpartum depression
- Why so many men avoid the doctor + how to get them to go
- Sink in + unwind with an Alvin Ailey dancer's stretch routine
- Mental health struggles inspired the momentous Oscar win
- The latest on Walgreens + abortion pills ban + boycotts
- We mourn the Mother of Disability Rights, Judy Heumann
- Here’s why + how nostalgia can help you get out of a funk
- Eek—a study shows parents lied about their kids + Covid
- 3-ingredient anti-inflammatory “brownies”? Yes, please!
Why doctors dismiss women's pain
Countless studies show how gender (+ racial) bias makes healthcare providers doubt women’s pain. Heart attacks happen. Epidurals fall out. A nurse subs Fentanyl with saline. Women scream. Their pleas are ignored.
Why does this happen?
Historically, medical studies have prioritized male bodies. If a woman’s symptoms don’t match (male) expectations, her experience gets dismissed. This education is slowly changing—the NIH now requires sex to be a variable in studies they fund. But in 2015, fewer than 35% of surveyed medical students felt prepared to address sex + gender differences at work. Until the system is overhauled, doctors + nurses will continue to underestimate women’s heart attack symptoms or prescribe them anxiety medication in situations where they’d prescribe men opioids.
Arm yourself with the personal stories + advice in this Washington Post article.
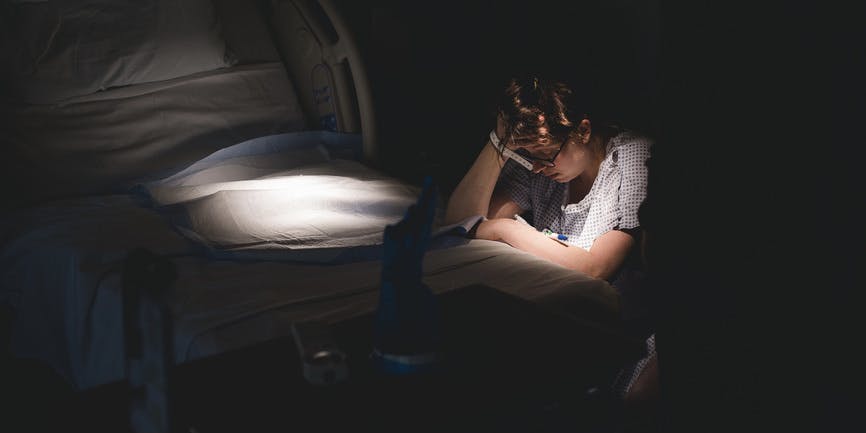
How to face medical PTSD

How do you cope when the thing that saved your life traumatizes you?
That’s the struggle for those with medical PTSD—the fallout of medical trauma that leaves us feeling a massive loss of control.
Unlike other forms of PTSD, medical PTSD triggers aren’t only external. Yes, a specific doctor, hospital visit or disinfectant smell can make us panic. But because our body was at the center of the trauma, internal triggers can set off the fight-or-flight response, too. Maybe a symptom that proved dangerous in the past returns. Or chronic illness uncertainty keeps us on constant alert. In response, we avoid medical care. Or we become hyper-vigilant + worry about any new sensation.
Those who’ve experienced medical trauma are at five times greater risk for PTSD than the general population. Read personal stories, studies, risk factor + coping tips in this Inverse article
No pain, more gain?

Anyone who’s run to the point of puking has chanted no pain, no gain, right? But trainers in an article from The Guardian are begging us to cut that out.
Sure, pushing beyond our comfort zone during a workout can boost our confidence. And we need to slightly embarrass our body to build strength, bulk up or train for a long-distance run. But beyond that, they claim that pain doesn’t help. Pushing miles or reps to the point where we can’t do one more can damage our sleep + immune system. Sometimes, we gain more when we slow down. Other times, doing rounds of low-intensity exercises throughout the day—what trainers call greasing the groove—can have the same effect as going hard all at once.
Read the article for more tips. Or shake up your routine with The Joy Workout.
Healthcare 411
The next stage of COVID is starting now (The Atlantic). Babies born today will likely contract Covid-19 within their first year or two, so we'll soon have generation of adults with some level of childhood immunity. This could mean that Covid-19 will eventually infect as often + mildly as the cold. But repeat infections could increase lifelong risk of chronic disease, too. As we’ve seen with the flu, commonality doesn’t negate the risk of death in adults. Also like the flu, vaccination reduces risk—but not enough children (or adults) get vaxed regularly enough to reduce those odds.
Is Medicare actually going bankrupt? (Vox). Medicare Part A is under threat. Covering hospital services + funded by payroll taxes, experts predict payroll taxes will cover only 90% of such costs by 2028 and the trust fund that makes up the difference will run dry. A total collapse has never happened before. But several factors—like the number of Boomers now enrolling in Medicare, increased hospital costs + a pandemic-affected economy—make this a giant puzzle to solve. Dig into the article for details
New York City rats can carry Covid variants, new study finds (The Guardian). Researchers found Alpha, Delta and Omicron Covid-19 variants in New York City rats. There’s no evidence that rats transmit the virus to people. But the study raises concerns about how circulation in urban animals may encourage new strains or variants that could then—somehow—pose additional risks. Great.
Topics
Sign up for the free Dr. B newsletter for a weekly report on the latest in healthcare + research-based advice for staying healthy and mentally well.